|
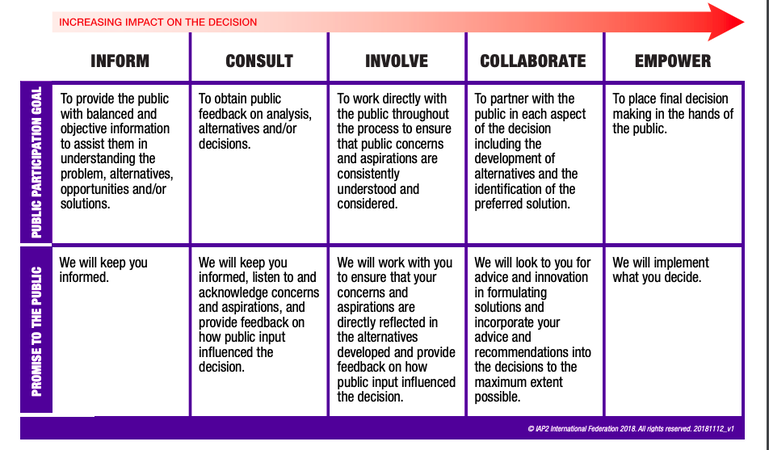
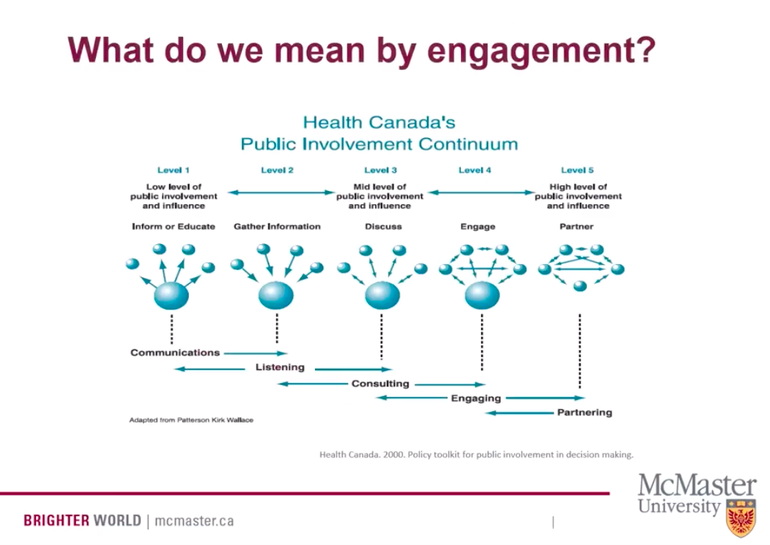
This past week has very much been ALL about patient and public engagement; where we have been, where we are and Are We There Yet? First up was listening to Carolyn Canfield's Top Ten Insights in Citizen Engagement (a Canadian perspective) during the McMaster Health Forum webinar. For those of you who don't know Carolyn, she is a pioneer in citizen engagement and patient safety, taking her tragic experience of losing her husband 8 days after surgery and redirecting that experience into deep impact around quality and safety of care in Canadian health care. Second, was watching Julia Ableson's presentation on Patient and Pubic Engagement; Are We There Yet? Dr. Ableson is the lead for the Public and Patient Engagement Research - Practice Collaborative also through McMaster. Third, was sitting in a board room with a fellow patient partner and one of our PhD researcher colleagues discussing supporting and building capacity in patient partners and researchers around patient orientated research. Now I am not terribly familiar with Dr. Ableson's work, however, a few things she shared resonated. And when I went to my meeting one thing popped up in regards to patient engagement and the IAP2 (International Association of Public Participation) spectrum of engagement that has been adopted by many in the world of patient orientated research and patient engagement. Julia actually used an older version of patient and public engagement and I didn't get a chance to ask her to share why. However, it became a focal point of my discussion later that day with my colleagues. One of the comments my PhD researcher had was that we should focus on Involve, Collaborate or Discuss, Engage. His reasoning was that there is no way we will EVER get PhD researchers to 'give up control' in order for us to reach Level 5, or Empowerment in the work of patient engagement. It took me a few minutes to wrap my head around that and then I remembered Dr. Ableson's image of the public involvement continuum. And I began to reflect on my own lived experience as a caregiver navigating the health care system for two decades. My experience, despite the gut wrenching loss of my daughter in the end, has been, for the most part, a good experience with little conflict or confrontation with the plethora of health care providers we encountered.
Sensing my colleagues resolve that empowerment is a 'nice to' but 'never will be' made me feel a bit deflated. But then I shared Dr. Ableson's version of public involvement and said, look at the image used of that far right level. All the balls are the same size. I challenged the notion of power and that IF power is the hurdle to empowerment then we need to redefine what empowerment means in the IAP2 model. What I think we need to start doing and articulating is that empowerment isn't about one stakeholder having MORE power over another; ie, patient over researcher, perhaps researcher over patient. Empowerment, in its truest sense, is ALL stakeholders having equity at the table, no one group has more power. And that true empowerment in patient and public engagement is about how all of us engage and interact together for the greater good; be it research, bettering health outcomes, designing health systems, or even at the basic level...alleviating pain and symptoms of a patient or loved one. Had I not had a true partnership with my daughter, Sophia's, health care practitioners and community support workers, I am not sure her journey would have been as 'good' as it was. And ultimately, she may have died experiencing a lot more pain and discomfort than she did. My challenge to both patient partners and those in health care (researchers, health care leaders, patient engagement specialists) is that Level 5 or Empowerment IS possible...if we all come to the table with equity. And what we come to the table with, is less about power and more about forging partnerships. Interestingly enough, Carolyn Canfield's presentation was symbiotic to Julia Ableson's despite both these presenters looking at patient and public engagement from two very different lens. Which kind of makes the point... As I embark on this new iteration of my life, professionally and personally, I am committed to working towards that Level 5 of Empowerment in order to impact change. I desire to build partnerships and am keen to learn and share. I am grateful that my PhD research colleague, despite our different lens, also became excited at this redefinition of Empowerment in the work we are just beginning. And I imagine we are going to do wonderful things together...that will have lasting, meaningful impact.
0 Comments
Last week I had the opportunity to attend BC Patient Safety and Quality Council’s Quality Forum in Vancouver as a patient partner. This was my first year attending and considering the forum was sold out in a mere three weeks, I was grateful. The Quality Forum is an annual conference, in its 7th year, featuring deep-dive sessions, presentations, and interactive workshops on a variety of topics related to improving quality across the continuum of care. In partnership with the Academic Health Sciences Network, I was invited to participate on one of the Pre-Forum panels discussing Learning Health Systems and the Critical Role of Engaging Patients with fellow patient partner, Chad Dickie and Ryan Sidorchuk, an engagement leader for BCPSQC. Stirling Bryan, Scientific Director for BC SUPPORT Unit, moderated. I was incredibly nervous participating in such an environment; being surrounded by influential health care leaders, academics upon academics, and clinical practitioners who share the front line journey alongside patients and their families. The event had over 900 attendees with patient partners making up approximately 2.5% of that. This year’s tagline was Activate, Integrate, Celebrate. It has taken me a solid week to really be able to think through and discern what themes, if any, I took away from the three day event. I can say with certainty that patient centered care was an influential theme throughout the event as was better health outcomes. Speaker Sir Chris Ham’s most positive take away from Quality Forum 2019 was patient inclusion…how great! That led me to think about my own experience in the health care system with my daughter, Sophia, and like a lot of caregivers and patients alike, we hope sharing our lived experience will impact health care delivery in positive ways. And as one prolific patient partner, Paul Caune, has coined…Hope is NOT a plan. However, I believe hope can evolve into purpose which can and does spur change. If we are to focus on patient partners in order to effect better health outcomes I think there are three distinct aspects of that; patient engagement, patient experience and patient equity. These terms mean different things to different people in different roles. However, for the sake of this blog, I am using the definition of patient engagement as set out by Fraser Health’s Awesome Handbook: ‘The term “patient engagement” is used in this handbook to describe patients participating in systems level planning. It is not used in the sense of patients being engaged in making decisions around their own individual care. “Patient” refers to a person who is currently a patient, has been a patient in the past, or is a potential future patient of health services, while “engagement” includes Ableson, et al.’s three criteria: 1) information about the issue is provided to the participants, 2) participants have the opportunity to discuss the issue amongst themselves and potentially with the decision maker, and 3) there is an explicit process for collecting the input from the participants.’ To reiterate, patient engagement is NOT ‘used in the sense of patients being engaged in making decisions around their own individual care.’ A common misunderstanding. Let me add I am also including patient families’ and informal caregivers in this conversation. Patient experience is the sum of ALL interactions that influence a patients perception across the continuum of care. So in my experience with Sophia this could entail appointments and procedures at our local Children’s Hospital. It could be our experience with Nursing Support Services, the Ministry’s At Home Program or even our interactions with our local pharmacists. Now here is where it may get prickly; patient equity. Not to be confused with health equity which amounts to offering all individuals the same chance to be healthy (that’s a whole other conversation!). If you were to search patient equity what comes up is patient capital. Patient capital is a term used in financial investment circles where an investor is willing to make a financial investment in a business with no expectation of turning a quick profit. Instead, the investor is willing to forgo an immediate return in anticipation of more substantial returns down the road. I am suggesting that the third leg in the better health outcome stool is this piece around patient equity or capital. Where we blend social and financial returns. What was evident at the Quality Forum is that there is a genuine desire to shift our health care system and delivery models to impact outcomes for ALL stakeholders. In putting a twist on traditional patient capital it is characterized by:
Speaker Rhona Flin discusses this ‘hurry up syndrome’ at a surgical level and how collective mindfulness and knowing when to slow down is as important if not more important than knowing when to speed up in practice.
After experiencing the rich content of Quality Forum 2019 and mixing that with my own lived experience as a patient partner, I am suggesting we need patient engagement, patient experience and patient equity in order to effect better health outcomes. Recognizing that patient equity or patient capital really is just my own minds way of trying to explain this piece around blending social and financial outcomes in the current system we have. How many times has a patient or family caregiver heard 'we don't have the resources for that' or 'you only have X amount of hours in nursing support', or 'X amount is covered, this amount is not'. It HAS to be a part of the conversation. In giving the final word to my daughter, Sophia, who died two years ago at the age of 16 to a complex disease process, “Take it Outside” (when referring to medical conversations in her room at the hospice), I think conferences like Quality Forum 2019 get us outside of our current thinking and open up our minds to alternative ways of ‘doing’. I am hopeful, I am full of purpose...that we can effect change together. B-HOPE: Better Health Outcomes through Patient Engagement, Patient Experience and Patient Equity |
AuthorBeverley Pomeroy is an awarded and highly sought after Community Engagement Strategist, Speaker, Author of Living Grief; The Profound Journey of Ongoing Loss. Beverley’s community service began with a fifteen year career in private health care working for MDS Inc (LifeLabs). This community health care role developed her acumen not only for serving people in need, but also her strength in business management and organizational renewal. Archives
December 2021
Categories |

 RSS Feed
RSS Feed